Let's Talk About Fetal Monitoring
Fetal monitoring is a birth preference that can have a significant impact on how you labor, so digging into the info to see what aligns with your preferences and needs is worthwhile. There are so many options when it comes to monitoring baby in utero, from intermittent monitoring to continuous monitoring and all the different machines to do so. Here at 615 Doula Co., education and having information before you need it is one of our top priorities. This blog post breaks down:
metrics fetal monitoring measures
pros and cons of continuous vs. intermittent monitoring
type of tools/machines used for monitoring
the electronic fetal monitor (most commonly used in hospitals) and what it all means
next steps for moving forward
Let's get to it!
What is Fetal Monitoring?
Fetal Monitoring is the act of using various types of instruments to help monitor baby during labor.
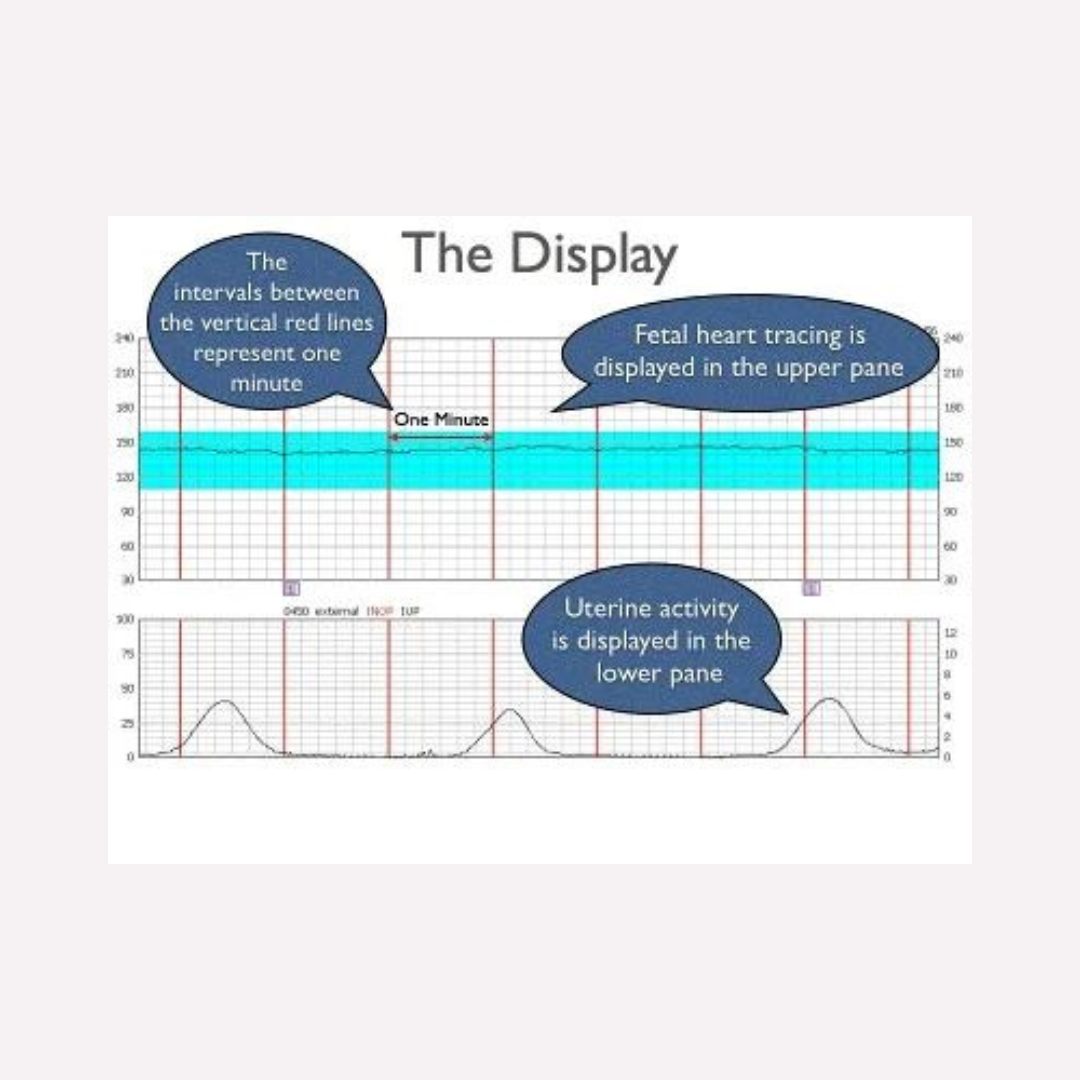
What Does Fetal Monitoring Measure?
There are four different metrics throughout labor. Not all tools/machines measure each one, but the four possibilities include:
Baby’s Heart Rate:
This is the main form of fetal monitoring, regardless of the type of monitor used (we will get into that later). It tells us how baby is handling labor.
The average fetal heart rate during labor is in the range between 110-160 beats per minute. Baby’s heart rate may vary by 5 to 25 beats per minute as baby responds to labor.Variability Pattern:
When monitoring the heart rate pattern, some accels (peaks) and some decels (valleys) are normal and this variability is a good sign. These accels and decels show baby is responding to contractions. However, persistently low dips can call for some changes during labor (i.e. positions changes, hydration like IV fluids, and further intervention if those don’t work).Contractions:
Some forms of monitoring also track pressure, i.e. contractions. When evaluating baby’s heart rate, knowing when the accels and decels are happening before/during/after contractions gives additional information to how baby is doing.
If utilizing an epidural, some epidurals cover the contraction sensation, so tracking contractions can be helpful in navigating your labor.Maternal Heart Rate:
Some forms of monitoring also track your heart rate. This can be useful, especially if the fetal monitor begins picking up on your heart rate (we don’t want that confusion because our heart rates are much lower than a baby’s). A persistently high heart rate might be a sign of a developing infection.
The Two Main Types of Monitoring: Continuous vs. Intermittent
When thinking about how you want to labor, one important choice to consider is what type of fetal monitor you prefer. Before choosing what type or tool you want used for monitoring, you first want to decide your preferences and needs for intermittent vs. continuous monitoring. As the words suggest, continuous monitoring is continuous, without breaks during labor. Intermittent monitoring checks in on baby at set intervals during labor (commonly every 30 or 15 minutes depending on the stage of labor). Continuous types of monitors (i.e. the Electronic Fetal Monitor, the Bluetooth Monica, etc.) and Intermittent types of monitors (a handheld doppler) both have pros and cons in their usage. Below, we lay out some pros and cons. Huge shoutout to Evidence Based Birth for being the brains behind these pros and cons. Check out their website here; they have amazing resources for all things birth.
Continuous Monitoring
Pros:
Lower rate of infant seizures
Some monitors are wireless and water-resistant
Can depict how baby is handling labor
Advised in higher risk labors
Advised if using epidural or Pitocin
Cons:
Higher rates of cesareans, and assisted (vacuum or forceps) deliveries
Restricts mobility of mom
Might restrict shower or tub use
Distracting or uncomfortable for mom (cords, straps, beeping, tethered)
Hospital personnel may be more focused on the monitor instead of mom
Intermittent Monitoring
Pros:
-Lower rate of cesareans, vacuum, and forceps
-Supports mobility and position changes (key for coping through unmedicated labor)
-Can be used in shower or tub
-Leads to more continuous, hands-on support from providers during birth
Cons:
-Higher rates of newborn seizures, though still rare regardless at .2%
-May not be appropriate for some high-risk pregnancies or those with complications
-Staff must be trained on how to log data instead of relying on machine that does it for them
-Requires 1:1 nurse to patient ratio to provide this hands-on care
Note: If your risk level changes during labor, your type of monitoring preferences may need to pivot.
Types of Fetal Monitors
1. Intermittent Doppler with Handheld Ausculation
Pros:
Intermittent Auscultation is evidence-based option for low-risk birth
Allows most mobility as the device runs on a battery and can go anywhere
Waterproof - can be used in the shower and underwater in the tub
More hands-on attention from nursing staff
Cons:
Staff have to know how to use it and how to chart the data
Requires frequent (commonly for the length of a contraction every 15-30 min) contact with medical staff and some patients prefer less or the hospital does not have a staff ratio to support this
Not recommended once some interventions begin (epidural, pitocin, etc.)
Image Credit: @emanating_kate on Instagram
2. Monica Novi Bluetooth Monitor
Pros:
Helpful for higher risk labors that require continuous monitoring
Wireless, no uncomfortable straps
Wireless, allows for more movement, within range of wifi
Usable in shower
Better reliability for higher BMI patients
Cons:
Continuous monitoring, associated with higher c-section rates in low-risk labors
To get the sticker patch to stick, skin is often roughed up with sandpaper
Sometimes there are connection issues with the wifi
Though many hospitals have, they are often limited
Bath usually not an option as signal doesn’t transmit through water well
Image Credit: @midwifeco.dfw on Instagram
3. Portable Mini Telemetry Unit
Pros:
Allows for mobility as it is powered by a battery pack
Allows for bath and shower as the pack is waterproof
Helpful for higher risk labors that require continuous monitoring (ex: on pitocin, but no epidural and still wants mobility and hydrotherapy)
Cons:
Continuous monitoring, so associated with higher c-section rates in low-risk labors
Not commonly available
Uses the traditional fetal monitoring straps so can be uncomfortable
Must carry the battery pack around on shoulder strap
Image Credit: gehealthcare.com
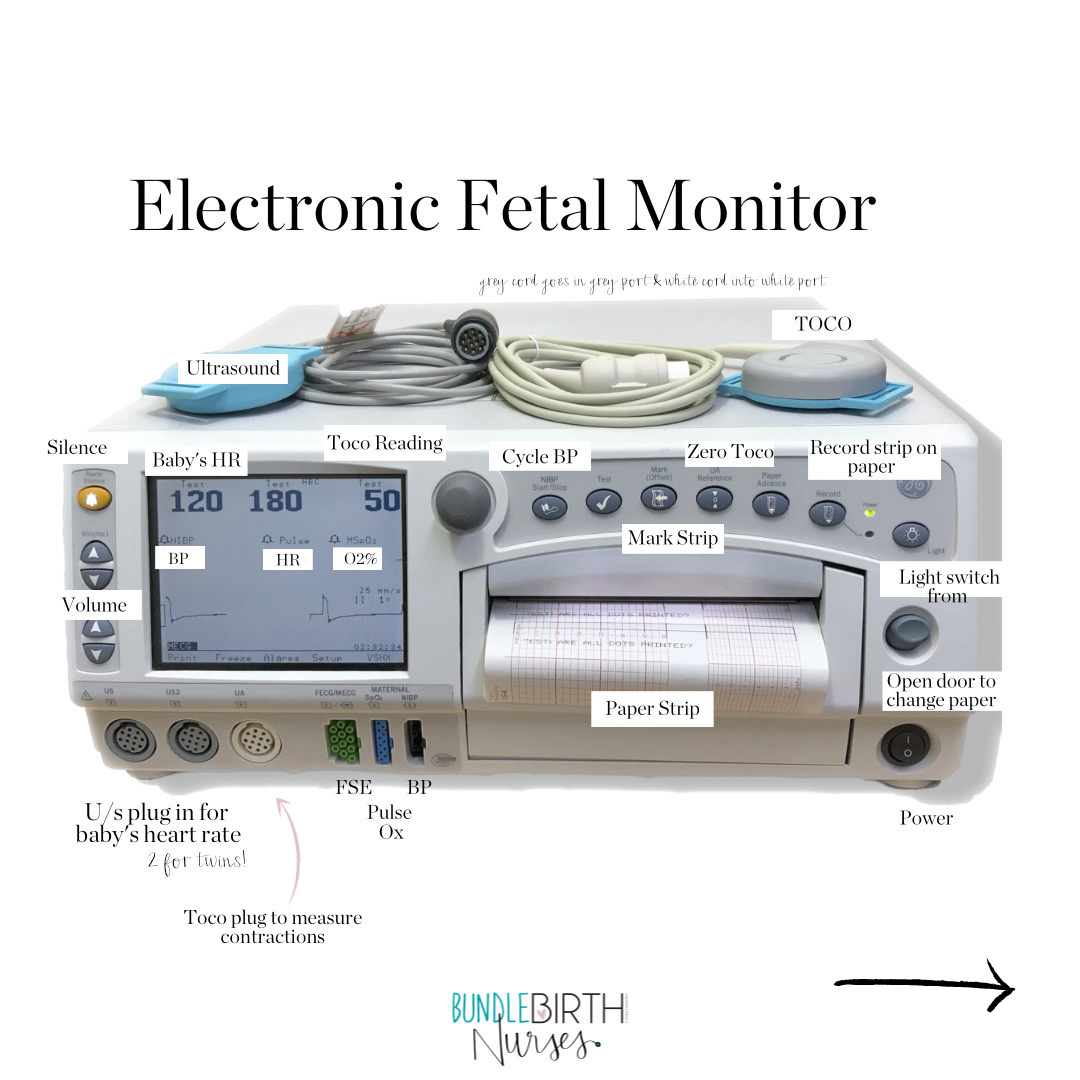
4. Electronic Fetal Monitor
This is the most commonly used monitor in the US. It is often the default option. Keep reading until the end to learn more about how to read the data this puts out.
Pros:
Readily available in all hospitals; logs data for staff and doesn’t require staff to be in room as often, staff most familiar with this technology
Continuous monitorings, so for higher-risk labors or labors with interventions like epidural, pitocin, etc.
Cons:
Restricts mobility by the length of the cord attached to the machine (in and around the bed)
Associated with higher c-section rates in low-risk labors
Straps are often uncomfortable
Often requires frequent adjustments by nursing staff
Image Credit: @heartsandarrowphotography on Instagram
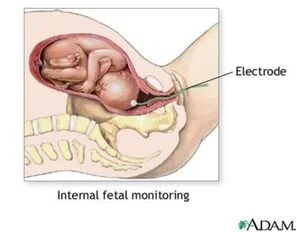
5. Fetal Scalp Electrode for Internal Monitoring
Pros:
Most accurate data on baby heart rate as it is connected to baby - should be reserved for very difficult to track situations that are showing concern
Cons:
Uncomfortable to place - inserted internally through cervix to baby
Electrode is a tiny corkscrew that punctures the baby’s skin; typically placed in scalp, but if baby is presenting a different body part this can be missed and puncture face or other part of body
Image Credit: Google Images
You Get to Choose
Fetal Monitoring is a birth preference. Of course, your preference may need to change or be shifted if your risk level changes during labor. However, always remember you do have a choice and knowing your options before birth helps to ease the mental load if you have any turns in the road during labor.
between continuous vs. intermittent monitoring
what type of monitor you prefer
Demystifying the Electronic Fetal Monitor
If you are planning to give birth in a hospital, this info on the electronic fetal monitor is important for you to understand what is going on in the labor room. The Electronic Fetal Monitor is most hospital’s default option and is therefore used in most hospital births. If you are planning for an unmedicated birth, you will likely want to choose another monitoring option, but having this basic knowledge in case of any pivots in labor, can be helpful. This monitor is also often used in triage, regardless of your preferences for medicated/unmedicated. If you are planning for an epidural or induction your chances of using this machine are much higher. Here is some basic info to demystify it.
Image by Bundle Birth Nurses
Image by Bundle Birth Nurses
If you are planning on using the Electronic Fetal Monitor
share this info with your birth team (partner and anyone you plan to have in the labor room)
and are without an epidural, know that you can still stand and move around as far as the cord will reach. Often the cart that the monitor is on can move too. Ask for a yoga ball to sit on or stand and sway, etc.
with an epidural, you can still move! There are lots of positional options for being in a bed, with the electronic fetal monitor, with an epidural.
ask questions about what things mean on this machine or the screen
request the beeping and heart tones to be muted
turn down lights or monitor / cover them if you are resting
the machine and data is interesting, but don’t allow it to become the focus of your experience. Remember to focus on how you are feeling, connecting with your baby and family, and communicating with your team.
Don’t forget, continuous monitoring is not evidence-based for low-risk labors that are unmedicated. If you do want/need continuous monitoring, you have other tool options.
A special thanks to Bundle Birth Nurses for these labeled images. You can check them out at https://bundlebirthnurses.com/ or on Instagram @bundlebirthnurses.